Judah from Maryland (Classical HCU, B6 Responsive)
A "Dinosaur" amongst us!!
Bringing better and deeper understanding to the complexities of HCU
A STORY OF TWO COUNTRIES
Half A Century Journey Living With HCU
February is Rare Disease Month, an important month for Homocystinuria (HCU). HCU is very rare compared to many other diseases. It is also quite complex as there are so many forms to this disease. I feel humbled and grateful to HCU Network America and Danae Bartke for allowing me to share my story in such an important month.
One needs to understand even though there are different types of HCU, there is a strong bond among all of us who have HCU. We may have different aspects of the medical disorder. However, in most cases we share some of the same core challenges and impacts. Many of us are on some kind of diet, take certain types of medication and are restricted with our protein intake. Some of the symptoms cross over to the various kinds of HCU, while others do not. Sadly, there is no cure. It might be very difficult to deal with the rigid aspects of the medical disorder. However, if one addresses these aspects; they can live a full and meaningful life. This was not the case a few decades ago. In general, due to the availability of special metabolic disease supplements and medications, people are living much longer.
This fall my sister, Avi, and I will be celebrating our 50th anniversary of diagnoses with HCU. In the early 1970’s, a diagnosis of HCU meant you were unlikely to live beyond young adulthood. HCU was just beginning to be recognized, research studies were scarce and very little medication was available to treat us. If it were not for Dr’s Naomi Amir, Gerald Gaull and Edward Rabb (see further on) things might have been a whole lot different for my sister and me. We owe them a debt of gratitude. They sure would have been proud to see how far we have made it in life.
Globally, the first cases of HCU were discovered in the early 1960's. In the USA cases started to be diagnosed in the mid to late 1960’s. Sadly, these cases were forms of what was called in the medical field in those days as “retardation”. In my opinion this labeling of the medical field for HCU showed great ignorance. To me the word “retardation” has a derogatory meaning and is a very harsh labeling. A better option would be physically challenged or slower than others. The early 1970's brought forth the first of research in the United States (though some was initiated in the 1960s).
My story is different and unique as it provides insight to medical information in conjunction with my story. I have experienced this firsthand. In addition, there are medical-scientific research that I have done on my own. This has the potential of being ground breaking and helpful to HCU patients. This information was reviewed by a well-known and respected HCU doctor. These discoveries have been supported to be true and accurate. In addition, these medical findings are supported by the National Institutes of Health (NIH) and can be found on their website.
There are many stories out there about HCU. I am not here to just to tell you another story, get pity or promote myself in any way. My goals are simple.
- HCU is relatively young orphan disorder. Note: I did not use the word “disease”. I did this on purpose. The word disease leaves such a bitter thought in our mind, a huge turn off, and finally it causes despair when you are at your lowest point.
- HCU is extremely difficult medical disorder, why you may ask? From my experience, HCU has so many different levels and parts to it. Unless one is truly an expert, certain aspects can be missed or misdiagnosed.
- Many people get diagnosed later in life. This makes things complex for the rest of their life as much of the damage has been done and is not reversible.
- I have been through the journey since early in its discovery. I want to pass the knowledge I’ve gained through my experiences to others. I also want to try to help them understand the challenges they may encounter.
- New parents will most likely not know what to look for or how to address their child’s medical issue.
- More information needs to get into the hands of patients so they 1) understand the type of HCU their kids or that they have 2) can set expectations both short and long term 3) take the appropriate steps to prevent further complications.
- More research needs to be done on older adults over the age of 40. We know some basics. However, as we age there is not much known about what to expect.
- A small group within Classical HCU might develop other medical issues. I will share and explain this a bit later. This will make it more challenging and difficult.
- More advocacy needs to be done so funds can be raised.
- Easier accessibility and cost-effective medication should be addressed. We need to push for less monopolies among vendors and distributors.
- Depending on where one lives one might need to travel long distances to see an HCU doctor.
- From my perspective, medical schools need to address deficiencies in education about rare disorders like HCU. However medical schools instead either brush these rare disorders under the carpet or limit students' exposure when addressing them in the classroom. This limits the students' knowledge base thinking that they may never encounter a patient with such a rare disorder. From my exposure to the medical world as well as almost fifty years with HCU (and other medical disorders) it evident to me that there is a great lack of doctor and other medical staff understanding of HCU. If medical students are not properly trained and educated in rare disorders, they will not be able to diagnosis and help patients especially in remote living areas or countries.
- Surgeons and other key staff who take part in the surgery need to better understand how to treat HCU patients during surgical procedure and post-surgery for any complications.
My story is very personal and complex since I have other medical conditions. Therefore, my story will differ from many other patients. I share my story with you because it is so important that you are aware of complications that other medical issues may impact managing HCU. Sadly, my doctors do not always know the best way to treat me. It becomes very frustrating for me. I am not one who gives up easily; I push my doctors to the limit and ask lots of questions. My father always told me questions are important and answers less important. However, in these medical issues both the questions and answers are imperative to survive. I am not always satisfied with the answers given to me by my doctors. Many times, I feel that my doctors are trying simply to get rid of me or push me off. Some doctors do not want to give credence to my discoveries. I terminated my relationship with many, many doctors over the years. These terminations are due to poor attitude and lack of help. I was not always satisfied with my doctors’ response or the way they handled certain circumstances. I believe many doctors over medicate you just to get you off their back.
In 1966, when I was two years old, my parents and I were vacationing in Yosemite National Park, when I became ill. After what seemed forever the hospital finally diagnosed me with appendicitis. Keep in mind appendicitis was not very well recognized in those days especially in this remote part of the country. By the time the hospital and team of doctors figured out what was going on, my appendix ruptured. This created even more complications. I was in an oxygen tent for quite some time post-surgery; I was just lucky to be alive. As proper records were not kept in those days, we will never know if HCU was a factor when I got sick.
My thoughts are that HCU did play a role. The reason for my theory is two-fold a) it impacts connective tissue. As evidence, my sister, who is almost 3.5 years my junior, as an adult had serious complications post her appendix surgery for many years. She still has flares up which are painful. b) HCU impacted my prompt diagnosis of appendicitis. No one thought to connect the dots in those days that maybe something serious was going on beyond a ruptured appendix.
At approximately the age of 4.5/5 years old I was having vision issues and started to wear glasses. Later in the life I developed some difficulty with my eyes (discussed later)
If HCU is not addressed in early stages, it could lead to poor motor coordination, clumsiness, and even developmental delays. In my younger years I was very clumsy and had poor motor coordination. I had a hard time catching a frisbee or a ball and even a harder time tossing, throwing, and catching. I could not keep my balance riding a bicycle. I ran poorly and was not able to keep up with my peers during gym time. My classmates were not kind.
In 1971 my parents immigrated to Israel, this was a longtime dream for my grandfather. Sadly, he passed away before he could travel there.
In 1966, when I was two years old, my parents and I were vacationing in Yosemite National Park, when I became ill. After what seemed forever the hospital finally diagnosed me with appendicitis. Keep in mind appendicitis was not very well recognized in those days especially in this remote part of the country. By the time the hospital and team of doctors figured out what was going on, my appendix ruptured. This created even more complications. I was in an oxygen tent for quite some time post-surgery; I was just lucky to be alive. As proper records were not kept in those days, we will never know if HCU was a factor when I got sick.
My thoughts are that HCU did play a role. The reason for my theory is two-fold a) it impacts connective tissue. As evidence, my sister, who is almost 3.5 years my junior, as an adult had serious complications post her appendix surgery for many years. She still has flares up which are painful. b) HCU impacted my prompt diagnosis of appendicitis. No one thought to connect the dots in those days that maybe something serious was going on beyond a ruptured appendix.
Israel in those days was much different than it is today. In 1971 Israel was a small, young country and was only 23 years old. As the country was in its infancy stages, it presented many challenges. These were the years before the Internet, mail between the USA and Israel took forever. The country did not have the ability or the knowledge to properly address HCU and no one was really in the field. So, what does one do in such a situation?
Injury leading to diagnosis
In 1972 as a young boy, I was playing on the porch of our apartment. There were two inflatable chairs. Too young to think of the consequences and wanting to have fun, I put these chairs one on top of the other. I then preceded to sit on top of them and they immediately toppled over. The after effect was not pretty. I hit my head and did not have a normal response as other children my age, which was to get up off the floor. I was rushed to the hospital and was there for several days. All kinds of tests were done including neurological and spinal tap to relieve pressure from my fall. I ended up with a concussion.
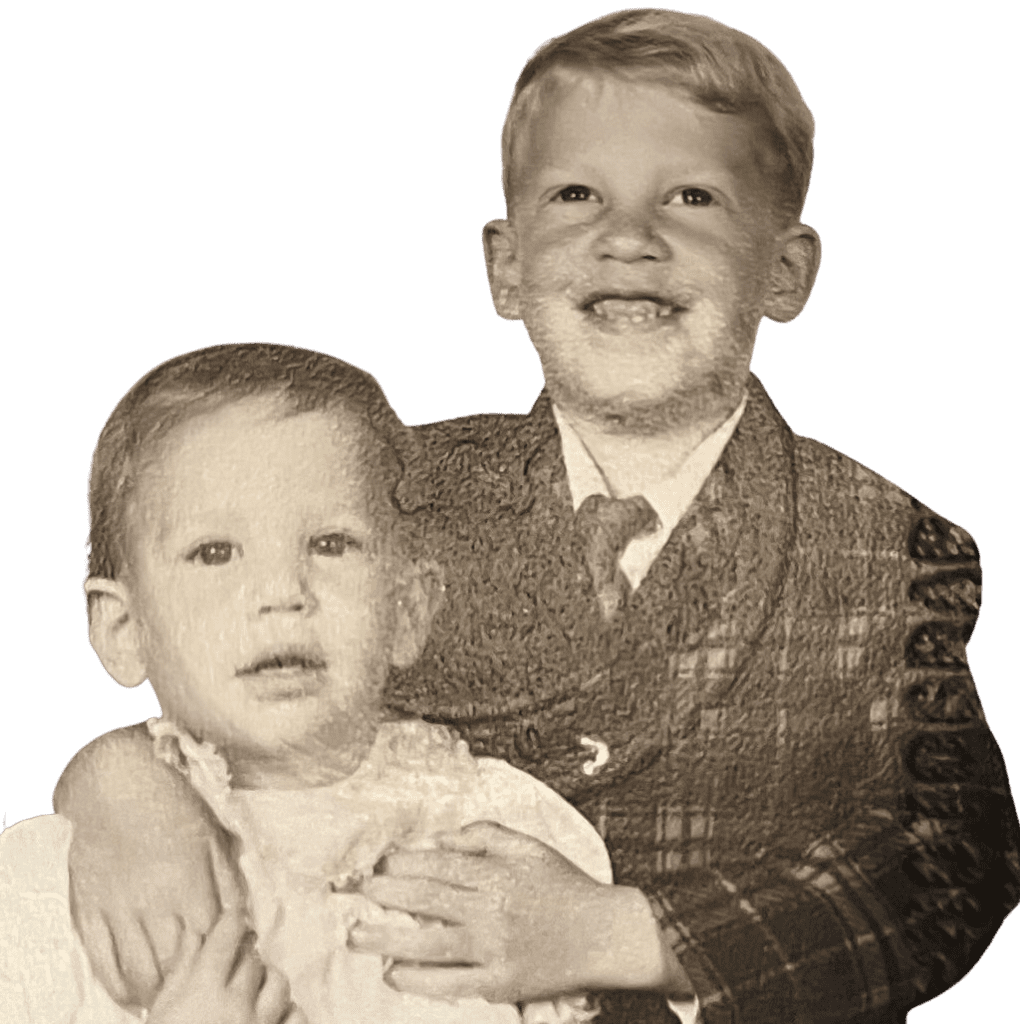
After I was released from the hospital my parents sought out a children's specialist in neurology. Her name was Dr. Naomi Amir, she was an American doctor who immigrated to Israel after medical school. She was a pioneer in pediatric neurology. In those days, Israel did not have many in field. She heard a lecture from the renowned Dr. Gerald Gaull, who was at the time an expert on HCU at Mount Sinai Hospital in New York City (NYC). My symptoms triggered a memory in Dr. Amir's mind. She remembered attending a lecture of Dr. Gaull many years earlier. Lots of blood work and neurological exams led Dr. Amir to believe I had HCU. She was in touch with Dr. Gaull who was doing research on HCU. Dr. Gaull was able to get a grant through National Institutes of Health (NIH) to cover all the expenses involved in flying my mother, sister, and I back to the United States. My sister, Avi and I became part of a group of pioneering patients.
Avi had no real symptoms, however, Dr. Gaull felt she needed to be tested. In the fall of 1972, we arrived at Mount Sinai Hospital in NYC for three months stay. Avi and I had much Genetic Testing in both Israel (before we left for NYC) as well as in the United States through biopsies. Keep in mind the United States was just starting to understand and intensifying its research on HCU.
During our 3 months stay at Mount Sinai Hospital our lives drastically changed forever. For the most part my sister and I were treated the same and no stone was left unturned. In an effort to better study HCU, Avi and I needed to make lots of changes. There was testing during the weekdays.
- X-Rays were taken of our skull, head, arms and back
- Neurological exams were done to see our reactions
- Eye examinations with renowned Dr. Edward Rabb to see the effect HCU had on our eyes (Dr. Rabb worked together with Dr. Gaull)
- Blood and urine lab work were done on a regular basis to check our numbers and see the impact on our protein levels
- Methionine loading was done several times to get a base level of methionine tolerance
- We were weighed every day to check the impact of the hospital diet we were put on for weight gain
- Psychological analysis and IQ testing were done.
- We met with our nutritionist Marsha. She sat down with us to explain what would happen during our visit. Special and restrictive low protein diet was developed. Our food was weighed before our meal. Our leftovers were weighed and recorded
- I had another spinal tap to get more scientific information
- Vitamin B-6 (pyridoxine) was added. This vitamin was the only thing identified we needed at that time. Additional medications were added later in life. I had Vitamin B-12, Folic Acid and Cystadane® added to my medication regimen when I was older
Conclusion to Dr. Gaull’s study
Both of us were diagnosed with HCU, were B-6 responsive, needed to continue our B-6 and low protein diet. In conjunction and consultation with Dr. Rabb, HCU impacted my eyesight. However, my sister’s eyes were not affected.
During these three months of inquiry, there were other patients of all ages and genders studied. There was another set of siblings. Some of these patients had various forms of HCU. However, my sister and I were the stars of Dr. Gaull’s success! We were the only ones who were B-6 responsive. He took great pride and joy in his work and the success in our progress. Dr. Gaull showed us off to other colleagues in the medical arena. At the time we were the only siblings whose reaction to treatment was the same. In the 1970’s, Dr. Gaull wrote several articles on his findings with my sister, me and other patients (who were part of this group) to share his findings with the scientific world.
Upon our return to Israel, until we moved back to the United States, we were medically followed by Dr. Amir.
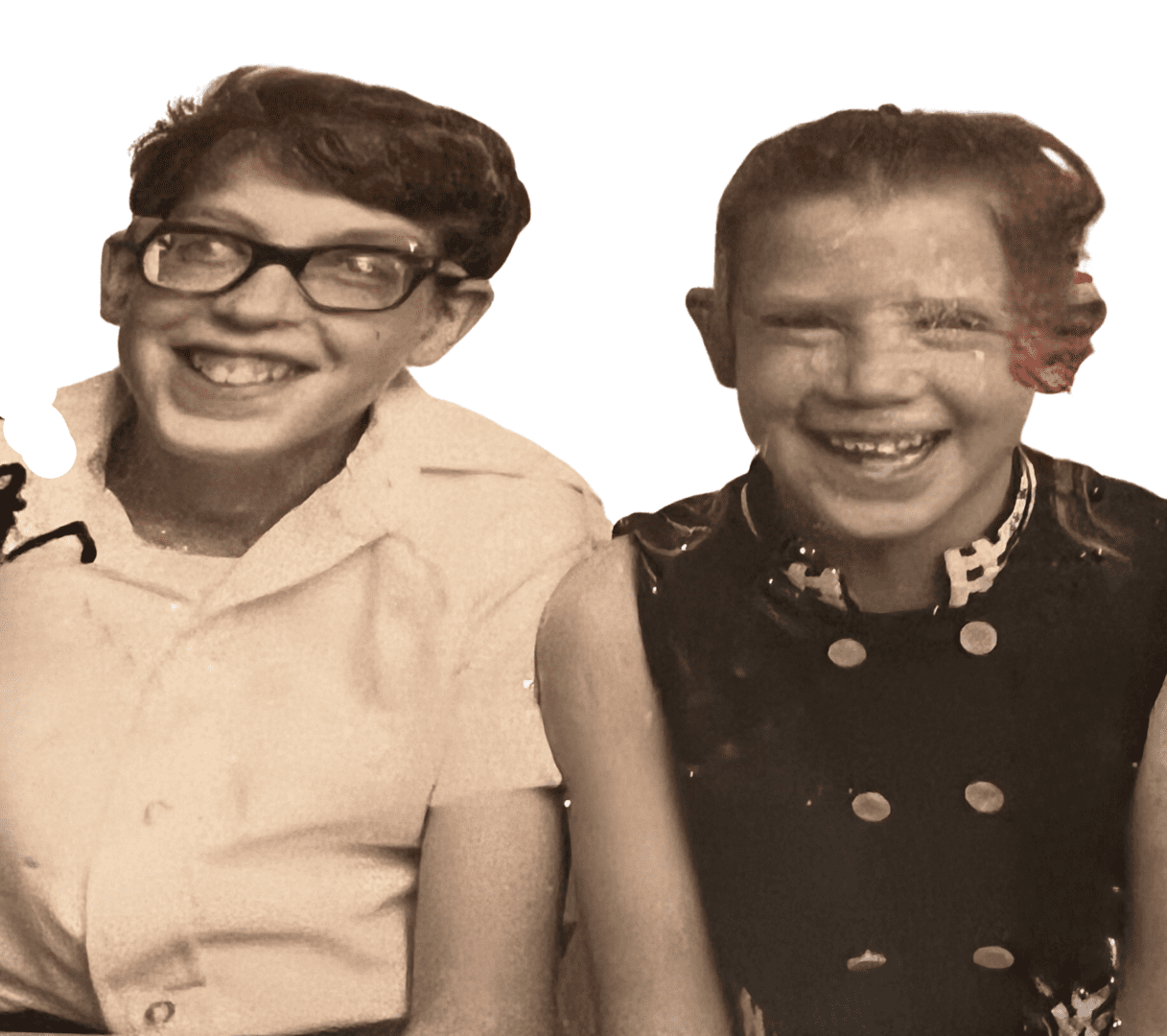
Avi did not have many changes until adulthood; however, I did. Upon our return from Mount Sinai my hair turned from blond to black. Avi’s hair was reddish (following our paternal grandfather). Avi’s hair became darker, but the reddish hair was still there. In her childhood, she was known as Gingi. Gingi is a Hebrew word for red head, it was very unusual to find a natural red head in those days.
In addition to the changes in my hair, my muscles and coordination had improved. In a short time, I was able to do things I could not do before. This included riding a bike, a major accomplishment for me.
Ophthalmology Challenges
By the mid-1970s, I was starting to have serious and more challenging eye issues. In early spring of 1975, I had an ophthalmic exam during which my doctor concluded that an emergency surgery was needed. At that same time, I had a serious case of dysentery. In those days Israeli hospital rooms were all open with lots of people and zero privacy. Prior to my surgery, the pre-op team was not up to speed on HCU. This upset my father deeply. He stopped the process until the doctors and the team involved with the surgery read up on HCU. My father called Dr. Gaull who returned his call from on top of a ski resort. The surgery was a success. My sister did not have any changes with her eyesight.
In the summer of 1975, we were visiting extended family in Baltimore. In an outing with them, I started to have severe pain in my left eye. We went to the Wilmer Eye Institute at John Hopkins University. Upon examination, the doctor told us that my lens dislocated and was blocking my vision. This was the root cause of my pain. They were able to get the lens back into place. On our way back to Providence, RI (where we were going to live for 18 months) we stopped by Mount Sinai Hospital in NYC to see Dr. Rabb. He concurred with the doctor in Baltimore. Once again, my lens subluxated and needed to be reset. I was put in a dark room to reset the lens. In the fall of 1975 once again, my lenses were subluxating. At that time, I needed special eye drops and needed to avoid dark places otherwise my lens would subluxate.
Later on, that year, Dr. Rabb did an iridectomy. It was a procedure of drilling a small hole in the right eye. In addition, he also adjusted my sight to allow one eye for long distance and the other up close for reading. This gave me relief from pain when the lens subluxated. In the fall/winter of 1976 upon our return to Israel, my ophthalmologist decided that it was time for my second lens to be surgically removed. From the late 1970’s until today my vision has been very good. Attempts to wear contact lens during my younger years and teen years were unsuccessful due to the sensitivity of my eyes. Therefore, I needed special glasses to compensate for my vision. In those days, lenses were very thick and hard to make. Fellow classmates were less than kind to me. Today glasses have come a long way with technology. In addition, in later years bifocals were added to improve my vision.
Decades later my vision has stayed virtually the same. In the last few years my eye pressure has gone up. I go to a specialist several times a year for checkups. I use special drops twice daily to bring the eye pressure down. One needs to be careful about eye pressure as it can result in glaucoma. If not addressed, blindness can occur. People with HCU have more chances of poor vison as they age.
In 1980 we moved back to the US, this time we relocated to Boston. At that time, my sister and I were under the care of Dr’s. Harvey Levy and Mark Korson. Both doctors are renown in the HCU field.
Back pain impacting my life
In the fall of my senior year of college, I developed severe pain in my back. The pain became so severe that I could barely get out of my bed. I needed to ask for medical leave from the university and extension on course work. After visiting several doctors including
Dr's Harvey Levy and Mark Korson, the decision was to do some exercises and pool therapy. This help to a degree. It took six months post university before things eased up. Over the years pain has come back but not as severe. Many of my family members suffer from severe back pain. It is possible that HCU played a role in this process. There was not enough scientific study to determine as factual.
Dental Challenges
I also have had challenges with dental and oral hygiene, such as crooked teeth, gum abscesses, more than normal cavities, crowded mouth (small palate) and overlapping teeth. This is not a well-described complication of HCU. However, I have heard from several other individuals with HCU that they have trouble too. I have had issues with crowding and numerous cavities, which resulted in me having to have teeth removed. In addition to that, I have an overcrowded mouth, overlapping teeth, which makes food more likely to be trapped and requires professional help to clean. To complicate dental care, I was told patients should also avoid laughing gas (nitrous oxide) during dental procedures because it increases homocysteine levels.
Overcoming Educational Expectations
Perhaps your story is similar to mine. My high school principal gave me grief over the thought that I would go to college. She told me not to go to college but trade/vocational school. She told me I would never make it in college. She really did not understand me very well. If she was only around during graduation to see how wrong she was. I received an award for English Composition during my high school graduation. In addition, I received a very high score on my Hebrew Achievements. I was a rebel and went to college. Due to my high grade on my Hebrew Achievement and good grades on my entrance exam to college, I was exempt from a year of Hebrew Language with a full 6 credits. In addition, I was on the Dean’s List for two years, which provided me full tuition. I was one of the few in my class to actually go to college and graduate. I needed to work harder than most students to succeed. It was not an easy road, but one with lots of challenges. Some of the challenges included lack of preparation of my high school for college and trying to advance myself in English as I spent most of my formative years in Israel.
Many years after college, I also went back to school for food service management and went on to graduate school until I was diagnosed with diabetes. Anything can be done if you put your mind to it. It might take a bit longer, but do not let others defeat your dreams or ambitions.
Getting older—new challenges
Over the decades, not much has changed with my HCU. In my late 40’s I needed to adjust a few things. This included a tighter control on my animal protein intake, adding certain medications and vitamins. At first it was challenging, as I was a meat and potato person. These days, the changes have become second nature. However, these changes were needed for the next chapter of my life. I eat a low protein diet with a limited animal protein diet. My HCU numbers have been very good since I made these changes. I have found that reading labels on food is extremely important. The more challenging issues were balancing HCU with other complex medical issues which also require a watchful eye on diet.
In the late 1990’s I developed diabetes. At first, I was diagnosed as type 2 (later on type 1). Oral medications did not work for me and needed to switch to insulin. Over the years, I used different types of insulin. These days, I am on large doses of both short and long-term insulin. Most people experience an increase in weight gain on insulin. I have been able to keep my blood sugar under better control. Over the last several years my Hemoglobin A1C levels (3-month blood work for diabetes) have been very good.
Over ten years ago, I had a blood clot. Blood clots are very common among HCU as well as diabetic patients. In addition, I also developed Rheumatoid Arthritis, osteoarthritis and monoclonal gammopathy of undetermined (M-Gus). Each are treated by different medical disciplines. If one studies or read about these medical conditions, there is much correlation and overlapping concerns. If one has these conditions, it puts them at a much higher risk for medical issues and complications. This includes blood clots, strokes, heart attacks and much more. I have discussed these concerns with my doctors but none of them will admit or discuss these overlying medical concerns. I am not aware of any studies or research done on these complex areas of disease therapy. Sadly, each medical discipline stands on its own. For over seven years I have been doing my own research. A few months ago, I looked at the NIH HCU website and found out that indeed symptoms of diabetes and RA can overlap and impact control of HCU. This was exciting news for me as this could lead to other possible breakthroughs. I confirmed my finding with my HCU doctor who supports my research.
In 2016, my life started to change completely. For a year I battled to keep my right leg. This included several surgeries and over 100 sessions of hyperbaric oxygen therapy. Hyperbaric chamber oxygen therapy can be very helpful in the healing process, especially wound healing. However, it is a time-consuming process which lasts several hours per session. During the middle of my second round with hyperbaric, I became very ill and was no longer able to continue with my treatments. After a year in wound care, being extremely ill and consultation with specialist, there was no other option but to amputate the leg. At that time, I decided I needed to resign from my work. This gave me time to focus on my deteriorating overall health. In June 2017 my right leg was amputated.
Initially there were lots of challenges and frustrations following my amputation. After several months of PT, I was able to get back my mobility. I needed to teach myself how to adapt to a new lifestyle, how to function back home, and within the community. In addition, I needed to adapt and re-learn how to drive with special hand controls. Over time it became second nature.
HCU is a connective tissue disorder which can complicate healing leading to delays and skin, which has lots of connective tissue, is particularly vulnerable. In February of 2021 once again things started to change. My amputated leg developed skin breaks down in the back of the knee and leg. Many amputees develop skin breakdown during some part of their life. However, that mostly comes from neglecting the remaining stump or wearing inappropriate supplies.
I have always been very careful with my amputated leg. I started to notice there was swelling on my amputated leg. Nothing was changing, and my concern was growing that this was getting too serious. I stopped using my prosthetic, so my leg could heal and used a wheelchair. I sent pictures to my leg specialist and he agreed with my assessment. He told me in four decades of working with amputees, he never saw anything like this. I called wound care right away. I have been doing wound care ever since. As my wound was healing, I developed fluid and infections. Tests and treatments were done but nothing was discovered as the root cause. Both my vascular doctor and cardiologist have cleared me of any major medical issues. In the meantime, I was released from wound care in October 2021. I feel like I am back to the drawing board trying to find the root of the problem and its solution. Until this is addressed, I am still in a wheelchair. Once this gets resolved, I hope to go back to Physical Therapy, so I get my life back on track.
Many lessons can be learned from this: you are not in control, your life can change very quickly, you need to learn to adapt to your new life and life is not always easy or rosy. When things look bleak or become challenging one needs to remember there are people out there in the world who are worse off then you. Over the last five years I have seen people who are in worse shape than me. The key is to continue to plug away and find solutions. Doctors do not always have solutions or the right answers. My sister and I have proven this time and time again. Both of us do not know the meaning of the word “no” and continue to fight to find answers.
In the last fifty years we as HCU patients have come a long way, however we still have a long way to go; more research is needed on older patients, cost of medications needs to come down and be more affordable. We need more options for medications and health insurance. Health insurance including Medicare and Medicare Advantage (all in one) programs need to be more welcoming and supportive. HCU needs to be better recognized like other diseases. The medical field globally needs a better understanding of HCU. HCU needs to be funded to keep helping patients. I am hoping the next generations will be more prepared and educated.
For a young family having a child with a genetic disorder like HCU can be overwhelming. I encourage parents who want to have children to have genetic testing to see if they are at risk.
In many cases, one needs to advocate for themselves or others or get someone to serve in this capacity. Getting into a support group will reduce the stress, provides a sense of belonging, gives a forum to share ideas and resources, and know you are not alone dealing with a tough situation.
I like to remind others with HCU that when one is sick (any kind of sickness), there is a trauma (including a wound) or an infection your HCU numbers will go up. (The same thing will happen if you are diabetic).
As I come to the end of my story, I want to recap some important information for those who are just starting the journey.
Important Note: Carriers of HCU may be impacted by HCU (especially if they are vitamin deficient). It could happen later in life. I think that carriers should have homocysteine levels checked, especially if they suffer from any clinical issues known to occur with HCU (e.g., blood clots).
Some lessons from my experience with Social Security and Medicare/Medicaid:
I hear from many how they cannot wait to be eligible for Social security and Medicare/Medicaid. I want to point out that access to these programs is not always a perfect experience. Social Security does not provide much to live on and Medicare, Medicaid, or both are very challenging to navigate (especially if you qualify due to a disability and are not at retirement age). I want to point out that it takes 24 months from when one starts to receive Social Security until one is eligible for Medicare and/or Medicaid. (As many of you know, receiving Medicaid is dependent on total household income.) It is important to know that if one does not accept Medicare when offered, one is financially penalized (if one tries to apply later, one can potentially lose out on other benefits). The options of Medicare for someone who is disabled is limited and not all things are covered. To improve coverage options, one can opt to go on an Advantage Program which has additional benefits. Advantage programs may not be available in all states and benefits might vary by states. Advantage programs are based on zip codes. There are potentially other choices like HMOs (but not all doctors accept these plans) or PPOs, but these may not be available in all states. No matter what you choose, one needs to review all options carefully and understand what is and what is not covered. Make sure all your needs are covered.
In conclusion, HCU can impact every part of your body. The most common areas of impact are the: Eyes, Skeletal, Central Nervous System, Heart & Blood (clots), and Connective Tissue. More detailed information on homocystinuria can be found on NIH Website and the HCU Network America website.
As HCU is a very rare complex medical condition, these medical professionals maybe suggested to be on your team of doctors:
- Specialist in HCU (Metabolic or Biochemical Geneticist)
- Primary Care Physician (PCP) (ideally someone with at least a basic knowledge of HCU)
- Ophthalmologist
- As needed or recommended (depending on your personal complications and medical history): Cardiologist, Hematologist and Neurologist
From my experience there are some high-risk procedures. I point them out to help you advocate for yourself, or your child. Make sure that your medical team is aware of the risk. If you need any kind of surgery (including outpatient) it is crucial that all staff involved in the surgery and during recovery, be aware that you are an HCU patient. Prior to surgery you need to make sure your surgeon talks to your HCU doctor to make sure they can make the surgery as safe as possible for you. Complications from surgery can happen to anyone, but especially HCU Patients. HCU patients sometimes have other potential complications. Therefore, providing your doctors and their team this information can make a real difference in the outcome of the surgery. For example, certain medications during and post-surgery can block your stomach from operating regularly post-surgery (doctors call this an ileus) and so you might not tolerate your Cystadane/betaine as well.
If one needs laughing gas (i.e., nitrous oxide) for dental teeth extraction, they should consult with their HCU doctor since this medicine can make your homocysteine increase.
Hospitals tend not to have all your medication, especially if they are specialty ones, or may not have your dosages available. At times your medication is changed with other similar medication and might cause your body to react differently. You might want to have a few days’ supply with you whenever you are in the hospital. If you have small scoops or measuring devices for your medication, make sure you remove from your medication bag and keep them in a safe accessible location as that they tend to get lost or forgotten to return by nursing staff.
Keep in mind everyone is different, with different results depending on when in life they were diagnosed.
Today all states in the US test for classical HCU when a baby is born (other forms of homocystinuria may also be identifiable by newborn screening at this time). However, newborn screening cannot always detect HCU (HCU America is working on improving this challenge). I would encourage parents with a family history of HCU to test their children once again at 2-3 years old. The earlier the diagnosis the better the outcome with less damage. As you can see from my history, my sister and I benefitted from diagnosis.
I am currently following a standard therapy. My therapy might differ from yours given our differences in age and co-existing complications. It is best if you work with your doctors and metabolic dietitians to reach your best results.
I hope my story is helpful to others as they start their journey with HCU. Best of luck!!
Never give up. Hoping that as scientists and doctors continue to work on HCU; they will find a cure for this challenging disease. Although Classical HCU does not have a cure if patients are addressed early and well maintained one can live a full and productive life.
Over a year and half ago I connected with the HCU Facebook group. My main reason I approached the group was great frustration with obtaining a reasonable price for Cystadane. I had been on it for several years prior. However, things drastically changed for me in September 2019 when I went from employee health insurance to Medicare.
I was fortunate enough to get a response from Danae Bartke, Executive Director of HCU Network America. There was an immediate connection with her. For the first time in all these years I had someone to talk to about HCU (besides my sister). Danae is much younger than me, however, she and I have seen and connected to many of the same doctors and have some of the same symptoms. Our HCU issues are very different (as described by Danae). Her brother who also has HCU reminded me of people I met half a century ago. Danae and I have had some phone conversation, email correspondences and private messages through Facebook for more than a year. Some of these communications were extensive and lasted several hours.
Danae' has a wealth of information, connections, resources, and very good knowledge of HCU. She responds very quickly and is very helpful to the HCU community. HCU Network America is lucky to have her as the Executive Director.
My HCU story is in honor of:
- Lisa Goldscheider, my wife who is always there to support and encourage me especially when medical issues become challenging.
- My father, Dr. Calvin Goldscheider on his 80th Birthday.
- Avi, my sister who has shared my journey for 50 years. I thank her for taking the time to read and give me feedback on my story.
- My HCU doctor’s past and present, whom Avi and I owe a debt of gratitude for following us for 50 years.
Added February 2022
